Immunity types
Innate
- Non specific, acts within minutes.
- Infection → pathogen recogintion by receptors → secretion of cytokines and interferons→ activation of cells to put up defences (eg inflammation) or die if infected, recruitment of white blood cells to stimulate long immunity → removal of infectious agent
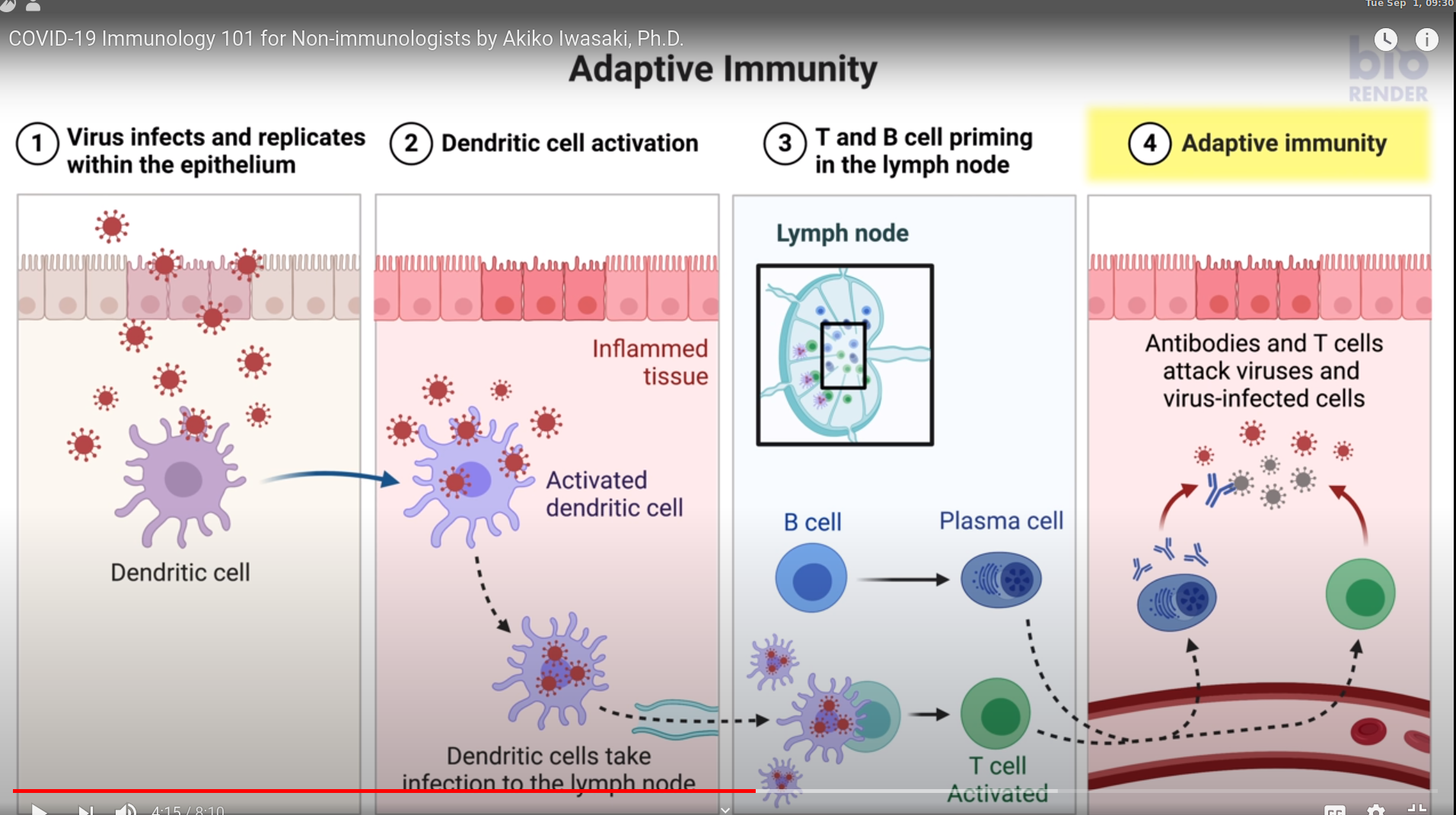
Adaptive
- Long term, specific. Takes a week or two to get going.
- Infection → Dendritic cells take infection to lymph nodes → Stimulation of T and B cells in lymphoid organs → Expansion and training of effector T and B cells → migration to infection site → removal of infectious agent
- Some B cells become plasma cells, which secrete antibodies for years.
- These antibodies can be used for detecting past exposure.
- Both T and B cells become memory cells and provide immune system for a long time (years), even after antibody levels are down. These can reignite defences later - Asymptomatic cases - less strong response, but much better than unprepped hosts.
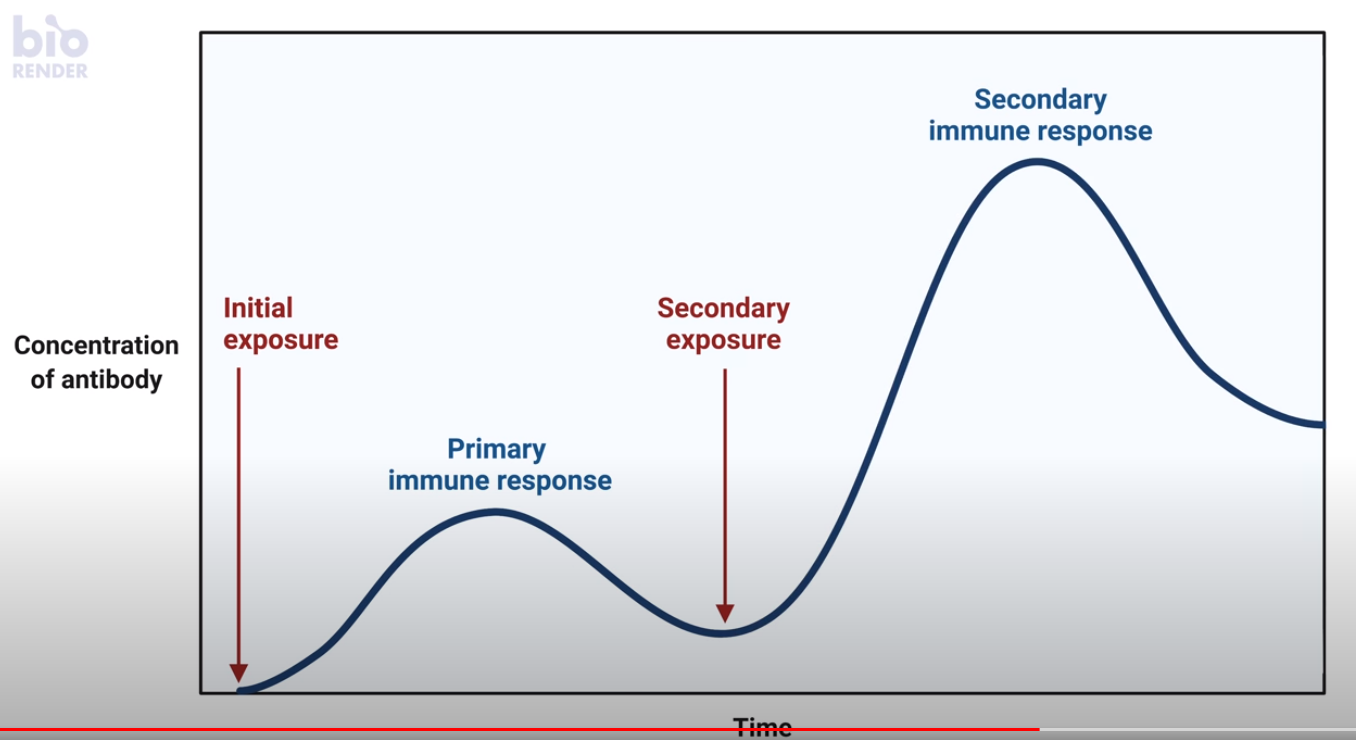
Antibody prevalance duration
- Measles - decades
- Common cold - 1/2 years.
- The level of Neutralizing antibodies vary from patient to patient.
- 32 individuals tested that were born in or before 1915 who had been exposed to the Spanish flu pandemic, each showed seroreactivity with the 1918 virus, nearly 90 years after the pandemic.
Herd immunity
When a big fraction of the population is immune (from vaccination?), germs cannot hop.
Cytokine storm
- From a chain reaction, more and more cytokines are sometimes produced.
- In case of wuhan virus, this results in inflammation, formation of fibrin and damage to lung cells, weakinging of blood vessels leading to seepage and drowning.